Indoor relative humidity is a function of seasonal climate and building HVAC. The range of 40 to 60% RH may reduce contagion and help those who are infected

Recent research explores the seasonality of COVID-19 (Hao, 2020; Araujo & Naimi, 2020) and the influence of relative humidity (Moriyama et al., 2020). However, it is the psychrometric overlap of climatic seasons and HVAC system operation that determines the indoor environment—where most viral propagation and human response occurs.
Research links air between 40 and 60% relative humidity (RH) with less-effective aerosol travel, shorter airborne and surface survival times, lower transmission rates (Noti et al., 2013; Marr et al., 2019; Wang et al. 2020), and more effective patient lung repair functions (Kudo, 2019). Patient respiratory benefits include less-viscous mucous membranes, more effective cilia-related and other antiviral actions in the lungs, and a more productive cough.
Yet hospitals in colder climates typically operate at lower RH levels (often 20%-30%) during winter, in line with minimum requirements. This is due in part to the risk of condensation on windows and in exterior walls, where moisture driven by an outward vapor pressure can damage building materials and cause other health problems.
However, most Northern Hemisphere cities have an immediate window of opportunity—before summer arrives—to increase humidification to 40%, largely without condensation limitations. By applying HVAC algorithms to representative weather records for major cities around the world, we identify opportunities and challenges for each climate zone. Below, we look at data for New York City.
Visualizing climate and windows of opportunity, challenge for NYC
New York’s first, and immediate, window of opportunity (indicated in green) is to increase humidification to 40% during the spring—even as COVID-19 is surging. After that, sufficiently humid outside air (gold) will keep indoor RH above 40%, while the dehumidifying effect of air-conditioning keeps it below 60%.
NYC’s second, but equally important, window of opportunity (green) is months away, allowing valuable time for humidifier and related upgrades before fall arrives (the season hit hardest by the 1918 influenza pandemic). As cold weather returns, RH will be of greater concern to facility managers due to the risks of condensation (gray boxes), while still allowing for stepped-down ranges of RH control with outdoor air approaching freezing (orange) and below freezing (white).
Visualizing climate for other cities
Other city climates vary widely from that of New York, and therefore represent different opportunities and challenges:
- View Climate Visualizations for US cities based on ASHRAE Climate Zones (PDF)
- View Climate Visualizations for other notable Northern Hemisphere cities (PDF)
- View Climate Visualizations for major Southern Hemisphere cities (PDF)
Note, Wuhan’s reported COVID-19 recovery aligned closely with the onset of humid weather. Tehran, like other cities in dry climates, will never reach that level of natural humidity, meaning it has a three-season window of opportunity. Miami and humid cities in the Southern Hemisphere require year-round air conditioning, with a risk of condensation in walls from moisture moving from the outside in.
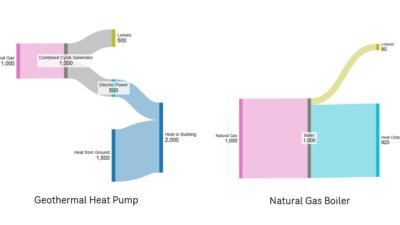
Humidification as a unique HVAC objective
Other HVAC design aspects—ventilation, filtration, air movement, space pressure relationships, temperature and purification—can help reduce contagion, and each is important (Wang, et al., 2020). However, no other HVAC aspect reduces contagion while also helping patients fight lung congestion.
Humidification’s relationship with building envelopes
While climate visualizations indicate representative areas for building envelope caution (gray boxes) and data to aid seasonal adjustments in RH setpoints (orange and white colors), we strongly urge facility managers to have their individual building envelopes evaluated for suitability with higher RH, using moisture migration programs or other means.
Recommendation for healthcare facility managers and engineers
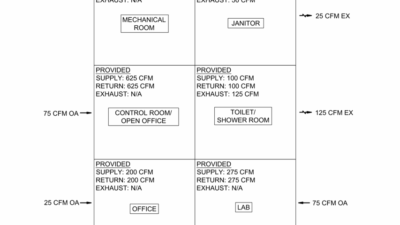
- Use immediate windows of opportunity to raise RH as close to 40% as possible, based on an analysis of building and system constraints.
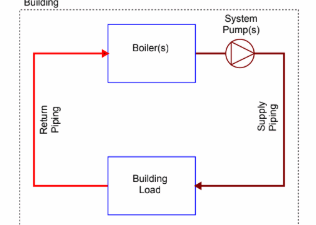
- Consider temporary reductions in economizer cycle operation to allow central humidifiers and any local boosters to do more.
- Optimize control and high-limit sensors for humidifiers at variable-air-volume air handing units.
- Before fall, consider adding booster or local humidifiers (steam, natural gas or electric, as appropriate), changing out or increasing capacity of humidifiers for economizer cycle mode, and possibly even enhancing glazing and wall systems.
- Before winter, step RH settings down incrementally to follow the weather (orange, white). Note, temperature can change faster than a building’s hygroscopic mass and system controls will allow.
- For temporary medical facilities and alternate care sites, consider how to get to 40% RH, even with novel means in an emergency model: e.g., RO/UV-treated water feeding atomizing-mist evaporative fans.
Implications for the future design of healthcare and other facilities
If building envelopes were designed and constructed to accommodate 40% RH throughout winter, we could help fight viral epidemics from the start of their typical season, not just towards the end.
We believe increased humidification will begin to drive design. Expect more triple-pane glazing with thermally-enhanced frames, robust vapor retarder systems properly placed within walls and roofs, local humidifiers and other changes with an integrated design approach.
As healthcare standard committees work through due processes for potential updates (some of us remember higher minimum RH standards), we are encouraged that ASHRAE has formed a new Epidemic Task Force to study these recommendations in more depth.
Much as 9/11 changed airport design, COVID-19 will change health facility design—and spill over into schools, workplaces and other types of building design and renovation (Reiman, et al., 2018; Taylor, 2019). However, the steps we have outlined are immediate and near-term interventions that can raise RH levels in accordance with specific climate zones, and perhaps slow the spread of this deadly disease.
This article originally appeared on SmithGroup’s website.
References
Hao, K. (2020, March 22). Warmer weather could slow the spread of coronavirus-but not by much. MIT Technology Review. Retrieved March 23, 2020, from https://www.technologyreview.com/s/615381/coronavirus-spread-could-slow-with-warmer-weather/
Araujo, M. B., & Naimi, B. (2020). Spread of SARS-CoV-2 Coronavirus likely to be constrained by climate. Preprint. doi: 10.1101/2020.03.12.20034728
Moriyama, M., Hugentobler, W. J., & Iwasaki, A. (2020). Seasonality of Respiratory Viral Infections. Annual Reviews, 2020. 7:2.1–2.19. doi: https://doi.org/10.1146/annurev-virology-012420-022445
Noti JD, Blachere FM, McMillen CM, Lindsley WG, Kashon ML, et al. (2013) High Humidity Leads to Loss of Infectious Influenza Virus from Simulated Coughs. PLOS ONE 8(2): e57485, https://doi.org/10.1371/journal.pone.0057485
Marr, L. C., Tang, J. W., Van Mullekom, J., & Lakdawala, S. S. (2019). Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. Journal of the Royal Society, Interface, 16(150), 20180298. https://doi.org/10.1098/rsif.2018.0298
Wang, Jingyuan and Tang, Ke and Feng, Kai and Lv, Weifeng, High Temperature and High Humidity Reduce the Transmission of COVID-19 (March 9, 2020). Available at SSRN: https://ssrn.com/abstract=3551767 or https://dx.doi.org/10.2139/ssrn.3551767
Kudo, Eriko & Song, Eric & Yockey, Laura & Rakib, Tasfia & Wong, Patrick & Homer, Robert & Iwasaki, Akiko. (2019). Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proceedings of the National Academy of Sciences. 116. 201902840. 10.1073/pnas.1902840116.
COVID-19 (Coronavirus) Preparedness Resources. (n.d.). American Society of Heating, Refrigerating and Air-Conditioning Engineers. Retrieved from https://www.ashrae.org/technical-resources/resources
ASHRAE Position Document on Airborne Infectious Diseases. American Society of Heating, Refrigerating and Air-Conditioning Engineers, 2014 (rev. 2020). https://www.ashrae.org/file%20library/about/position%20documents/airborne-infectious-diseases.pdf
Reiman, J. M., Das, B., Sindberg, G. M., Urban, M. D., Hammerlund, M. E. M., Lee, H. B., … Pierret, C. (2018). Humidity as a non-pharmaceutical intervention for influenza A. Plos One, 13(9). doi: 10.1371/journal.pone.0204337
Taylor, Stephanie, Tech Hour: Occupant Health, Building Energy Performance and Humidity (December 19, 2019). Available at https://www.youtube.com/watch?v=4jCji-mIKVQ