Ventilation and indoor air quality play an essential role in providing an initial line of defense to protect patients and staff and minimize infection risks in health care facilities.

Learning objectives:
- Understand the relationship between ventilation, indoor air quality and infections in health care facilities.
- Identify the codes, standards and best practices guiding ventilation design in health care facilities.
- Explore real-world examples of effective ventilation strategies for health care and understand the risks of inadequate indoor air quality.
IAQ insights:
- Indoor air quality (IAQ) plays a critical role in preventing health care-associated infections (HAIs), which remain a leading cause of death and financial burden in U.S. hospitals.
- Strategies like ventilation, filtration, humidity control and UV disinfection can directly influence patient safety and infection control in health care environments.

Despite being largely preventable, health care-associated infections (HAIs) remain a persistent and costly issue in the U.S. health care system. According to the National Institutes of Health National Library of Medicine, approximately two million patients suffer from nosocomial infections in the US, with nearly 90,000 of those estimated to die. This makes HAIs a top-five leading cause of death in US acute-care hospitals. Beyond the devastating human toll, the financial burden is staggering. It is reported that overall annual direct medical costs of HAI to U.S. hospitals range from $28 to $45 billion. While infection control is often associated with hand hygiene and operational protocols, engineers have a direct and powerful influence on patient health through ventilation and indoor air quality (IAQ) measures.
Health care design aims to minimize airborne infection risks in critical environments such as intensive care units (ICUs), operating rooms (ORs) and oncology suites, while ensuring that airborne pathogens remain contained in isolation areas. Proper ventilation strategies not only shield vulnerable patients but also protect health care workers from exposure to airborne contaminants. Ultimately, our role as engineers extends beyond system performance — we are a frontline defense against infection and contribute to safer, more effective health care environments.
Understanding the history is crucial in recognizing the severe consequences of neglecting IAQ in critical health care spaces. One of the most sobering examples is the tragedy at the Roswell Park Bone Marrow Transplant Unit in Buffalo, New York, in 1982.
In mid-1981, the New York State Department of Health, which operated the hospital, requested funding for heating, ventilation and air conditioning (HVAC) system upgrades. However, the funding never materialized, and despite outdated ventilation infrastructure, the hospital proceeded with opening a new Bone Marrow Transplant Unit in 1982.
Over the next eight months, more than one-third of the unit’s patients developed invasive aspergillosis and died, ultimately leading to the unit’s closure. Investigations later revealed an alarmingly inadequate air quality environment for highly immunocompromised patients. The unit was equipped with only 10% efficient, roll-type filters, grossly insufficient for filtering out airborne contaminants. Compounding the issue, heavy construction adjacent to the hospital stirred up fungal spores, introducing contaminated air into a space already lacking proper air treatment measures.
This tragedy underscores a fundamental truth: IAQ is not just a design consideration — it is a matter of life and death for patients in critical care settings. The lessons learned from Roswell Park emphasize the non-negotiable need for high-efficiency filtration, robust ventilation strategies and strict airborne infection control measures in health care facilities.
Air changes and infection control
The management of air change rates in patient care areas is a fundamental pillar of infection control in health care facilities. Air changes per hour (ACH) refers to how many times the air within a space is replaced or recirculated each hour. Research shows that insufficient ventilation increases the risk of disease transmission, making high ACH rates essential in areas with elevated infection risks.
Increasing the air change rate serves two critical functions:
- Diluting airborne contaminants, which reduces the concentration of pathogens in the air.
- Removing harmful particles more quickly, protecting patients, staff and visitors while preventing the spread of infections to adjacent areas.
There are two primary types of ACH:
- Total ACH: The number of times the entire air volume in a space is replaced per hour, whether with recirculated or outdoor air.
- Outdoor ACH: The number of times per hour that the total air volume is replaced by fresh outdoor air.
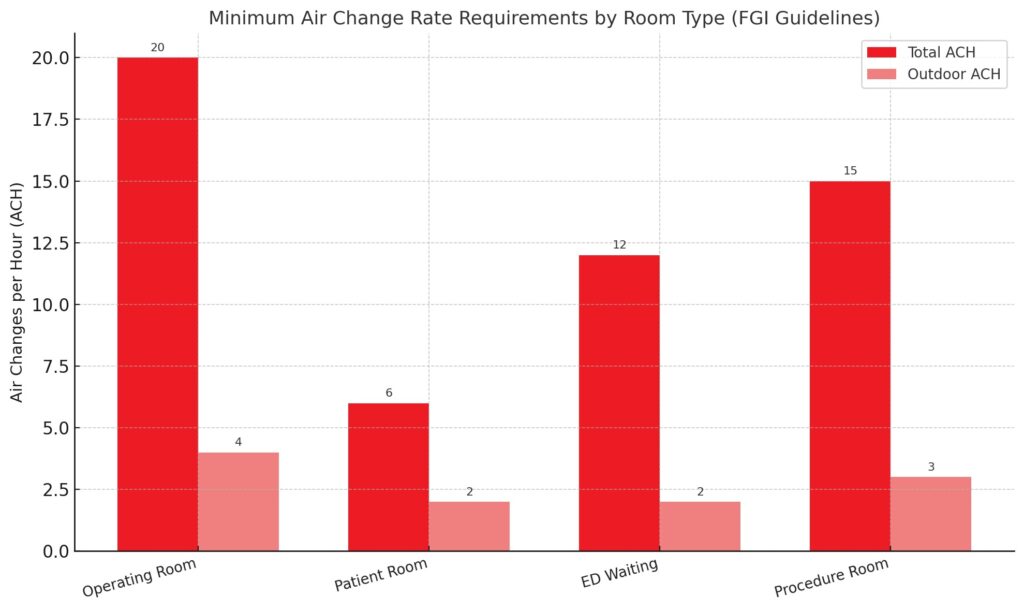
For reference, a typical patient care space requires six total ACH and two outdoor ACH, meaning at least 33% of the air supply must be fresh outside air to meet the minimum ventilation requirements. However, more sensitive areas — such as ORs, isolation rooms and ICUs — can often require total ACH rates up to 20 or higher, depending on the facility’s specific needs.
The primary standard governing ACH requirements by space type is the ASHRAE Standard 170: Ventilation of Health Care Facilities. Table 7-1 within ASHRAE 170 outlines the minimum requirements for total ACH, outdoor ACH and exhaust air for various health care spaces. The Facility Guidelines Institute (FGI) has formally adopted ASHRAE 170 into its health care design standards, making compliance mandatory for all hospitals in the United States.
Additionally, state and local health care codes may impose stricter requirements. States such as California, Texas and Florida are particularly known for enforcing their own health care ventilation standards. Designers must ensure compliance with both national guidelines and local amendments.
While high ACH rates are essential for infection control, strategic air change setbacks can improve energy efficiency without compromising patient safety. Spaces such as ORs, which require very high ACH rates when occupied, may allow for reduced ACH rates when unoccupied, significantly lowering energy consumption while maintaining compliance with safety standards.
Filtration: Line of defense
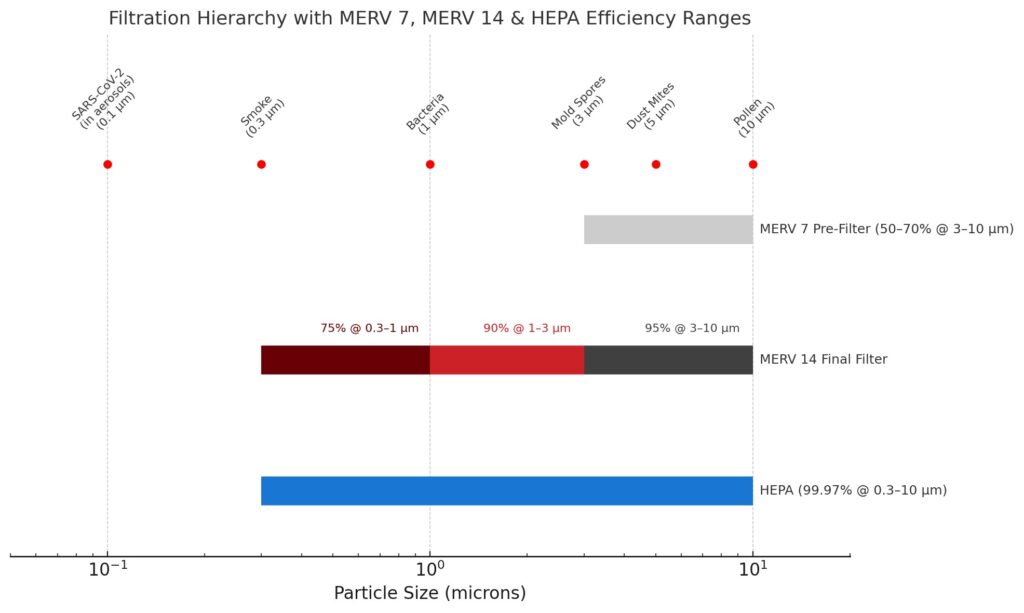
Filtration is another fundamental design consideration in airborne pathogen mitigation. Air filters, composed of fibrous or porous materials, capture particulates and microorganisms as air moves through the HVAC system. Properly selected and strategically placed air filters can effectively remove smoke, dust, pollen, mold, viruses and bacteria, significantly improving IAQ and protecting patients, staff and visitors.
Filter effectiveness is measured by the Minimum Efficiency Reporting Value (MERV) rating system, based on the testing methods outlined in ASHRAE Standard 52.2: Method of Testing General Ventilation Air Cleaning Devices for Removal Efficiency by Particle Size. A higher MERV rating indicates a greater ability to capture smaller particles. ASHRAE 170 Table 6-4 specifies minimum filtration requirements for different health care spaces. In most patient care areas, two stages of filtration are required to ensure optimal air quality:
- Pre-filtration (first filter bank):
- Located at the air handling unit (AHU) intake.
- Uses a low-MERV filter to capture larger particles from the mixed airstream.
- Protects AHU coils and components from debris buildup.
- Final filtration (second filter bank):
- Located downstream before air is supplied to occupied spaces.
- Uses a high-MERV filter to remove finer particulates, ensuring cleaner air delivery.
Certain high-risk health care environments, such as protective environment rooms, surgical suites and bone marrow transplant units, require high-efficiency particulate air (HEPA) filtration with a MERV rating of 17 or higher. HEPA filters are designed to trap 99.97% or more of airborne particles as small as 0.3 microns, offering the highest level of protection against airborne pathogens.
Even the most advanced filters are ineffective if air bypasses them due to poor sealing or improper installation. Filter frames play a crucial role in ensuring that all air passes through the filtration system. Modern filter banks use metal frames with gaskets or seals, creating a secure seal that minimizes air leaks and bypass.
To prevent microbial growth and contamination:
- Never use wood as a filter bank framing material. Its porous nature retains moisture and promotes microbial growth.
- Regularly inspect and maintain filters to prevent debris buildup, which can introduce contaminants into the airstream.
- Ensure proper sealing to eliminate gaps, which have been linked to HAIs, including aspergillosis outbreaks in immunocompromised patients.
By implementing effective filtration strategies, health care facilities can create a safer environment, reducing infection risks while maintaining high indoor air quality standards.
Humidity control
Humidity is often associated with comfort and convenience, but its impact extends far beyond occupant comfort. Relative humidity (RH) may play a direct role in infection control within health care environments.
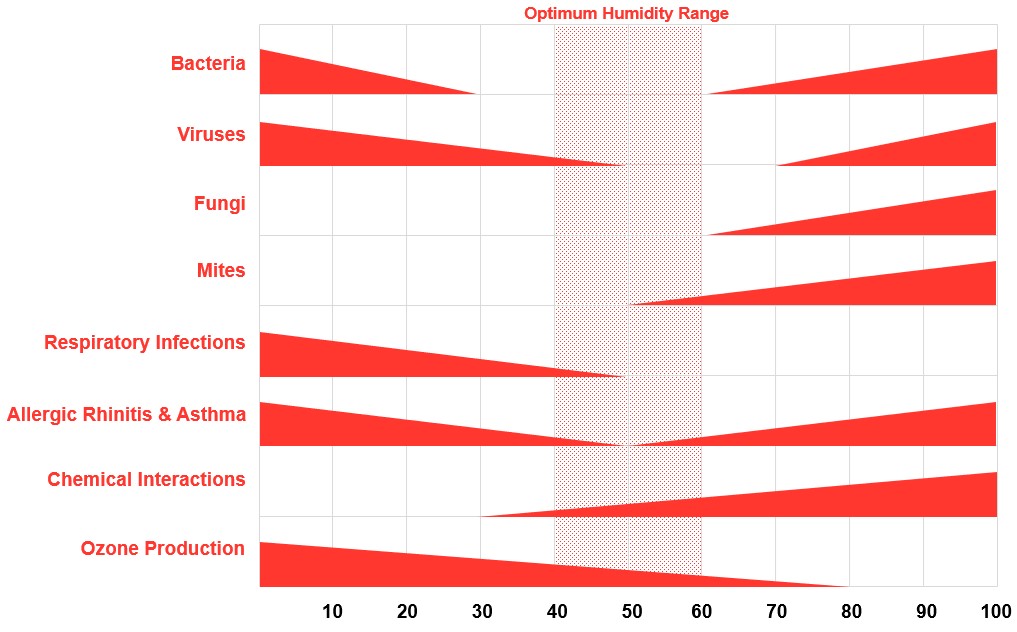
The paper “Indirect Health Effects of Relative Humidity in Indoor Environments” (Arundel AV, 1986) introduced a pivotal tool in infection control: the Sterling Chart. This chart compared the survival rates of bacteria, viruses and fungi across different RH levels. One of its key findings was that the influenza virus became less viable as RH increased above 40%, but virus survival rates spiked again when RH exceeded 60%. This trend was observed across multiple airborne pathogens, leading researchers to determine an optimal RH range of 40-60% for minimizing infection risks in health care settings.
Excess humidity (>60% RH) creates an ideal environment for fungal growth. Fungi such as Aspergillus and Candida, commonly found outdoors, can infiltrate indoor spaces when conditions allow. High humidity levels can cause sweating on exterior walls, especially in cold environments, promoting mold growth if proper architectural and mechanical design considerations are not taken. In health care facilities, this mold contamination can become a serious threat, especially for immunocompromised patients.
On the other end of the spectrum, excessively dry air (<30% RH) can be equally hazardous, particularly for vulnerable patients. Low humidity:
- Weakens the respiratory immune system, making individuals more susceptible to infections.
- Increases airborne pathogen survival, allowing viruses and bacteria to remain suspended in the air for longer periods.
- Reduces particle settling, meaning infectious aerosols stay in the breathing zone instead of settling out of the air.
By maintaining RH within the recommended 40-60% range, health care facilities can enhance respiratory immune defenses, reduce airborne pathogen survival and create a safer indoor environment. ASHRAE Standard 170: Ventilation of Health Care Facilities provides minimum and maximum RH requirements for different health care spaces. Engineers should also reference state and local jurisdictions, as they may have more stringent humidity control regulations.
Ultraviolet light technology: Enhancing air quality
As health care facilities adopt innovative approaches to infection control, ultraviolet (UV-C) light has become a proven solution for reducing airborne and surface contaminants. UV radiation disrupts the DNA and RNA of microorganisms, effectively reducing bacteria, viruses and mold concentrations.
It’s common to see UV-C technology within AHUs, positioned downstream of the cooling coil. This placement prevents microbial growth on damp coil surfaces and sterilizes air before it is distributed. A UV intensity of seven watts (W)/square foot is sufficient for coil maintenance, while 20 W/square foot is recommended for airborne pathogen reduction.
Beyond HVAC systems, UV disinfection is also used in operating rooms and critical care areas to sanitize surfaces and air between procedures. When properly implemented alongside filtration and humidity control, UV-C technology adds a powerful layer of defense against health care-associated infections, reinforcing safer environments for patients and staff.
Pressurization and airflow patterns
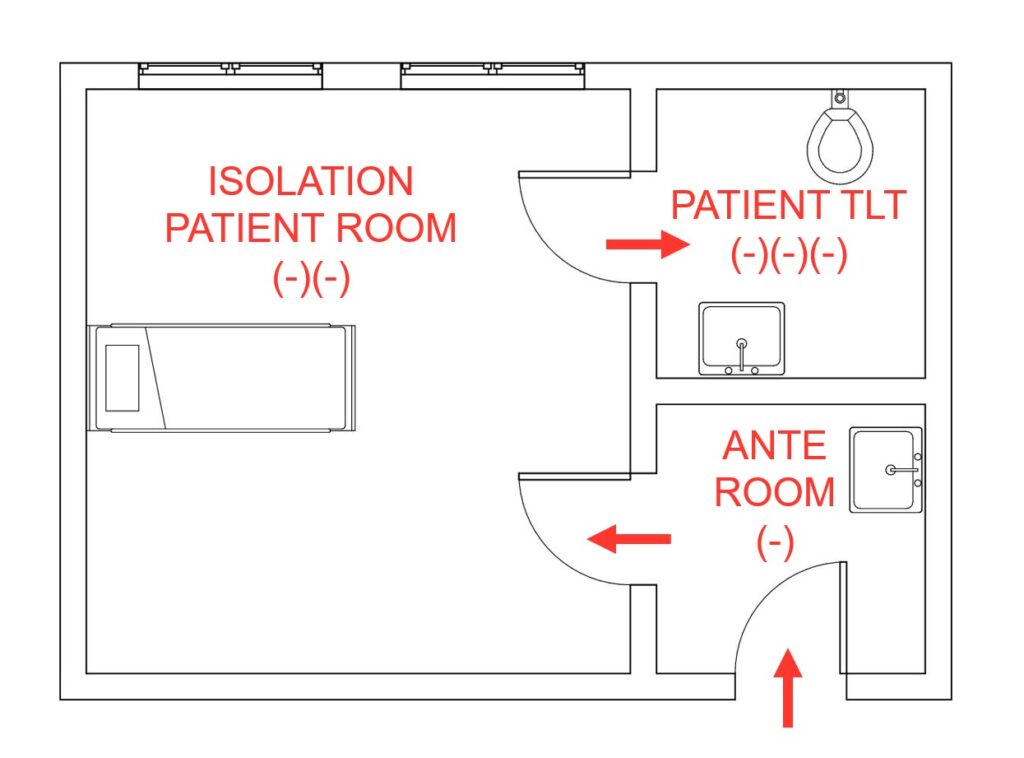
Proper airflow design, including positive and negative pressurization, plays a critical role in reducing infection risks by controlling airborne pathogen movement within patient care zones. Positively pressurized spaces are considered “cleaner” and prevent airborne contaminants from infiltrating, while negatively pressurized, or “dirtier,” spaces help contain and exhaust contaminants safely. ASHRAE Standard 170 outlines the specific pressurization requirements for various health care environments.
Table 7-1 in ASHRAE 170 provides detailed airflow and pressurization requirements for different hospital room types. For example, ORs must maintain positive pressure relative to adjacent spaces to keep contaminants out, whereas public waiting areas in emergency departments require negative pressure to prevent the spread of airborne pathogens to other areas of the hospital.
Pressurization is just one aspect of airflow control in health care design. Another critical factor, addressed by the FGI, is the airflow pattern within a space.
Laminar airflow (LAF) systems generate a smooth, unidirectional flow of filtered air over the surgical table, creating a protective air curtain. The air is directed downward, shielding the surgical site, and is then efficiently removed through low-level return grilles positioned on opposite sides of the room. This design helps control airborne particle movement, reducing contamination risks and enhancing patient protection.
Airflow management at return grilles is an often-overlooked aspect of contamination control. During final system balancing, supply airflow remains constant while return airflow is reduced to achieve the required positive pressurization. This reduction in return air velocity can compromise contaminant removal efficiency if not properly accounted for in the design. Ensuring that return grilles and ductwork are adequately sized is essential for maintaining effective contaminant control and meeting pressurization requirements.

While codes and standards provide essential design guidelines, designers must understand the underlying principles behind these requirements. The goal of health care ventilation design is to protect patients and staff by minimizing infection risks through strategic airflow management.
A shared responsibility in health care design
Health care designers, engineers and facilities professionals must actively engage in conversations about patient care operations and environmental risks. Are immunosuppressed patients housed in these areas? Will there be construction activity nearby that could introduce airborne contaminants? While we can’t predict every challenge, we can design proactive solutions that minimize infection risks and protect both patients and staff.
Environmental contamination is often an unseen threat. Fungal intrusion, for instance, may originate within HVAC equipment, especially if moisture accumulation and periods of stagnation allow microbial growth to flourish. Designers must anticipate risks, ensuring that humidification systems are managed properly and integrating HEPA filtration at critical points, such as directly at air grilles in high-risk patient areas.
The Roswell Park tragedy serves as a powerful reminder of the devastating impact of poor IAQ, particularly in environments where immunocompromised patients reside. Construction and renovation activities can dramatically increase airborne fungal concentrations, emphasizing the need for stringent pressurization control, advanced filtration and continuous air quality monitoring.
Understanding that decarbonization and energy efficiencies are becoming more critical for the outdoor environment, the need for ongoing research on the relationship between infection and certain design considerations is greater than ever. Routine IAQ checks should become a standard component of health care facility maintenance, ensuring that ventilation systems perform as designed. It should be our job as designers to create systems that are easily maintainable by the facilities staff. Maintaining a safe environment is a collective responsibility, requiring collaboration between doctors, nurses, infection prevention specialists, facility engineers and designers.
Ultimately, every design decision should be guided by a simple but critical principle: “Do the right thing.” Does this design protect patients and staff? Does it mitigate risk? As health care engineers and designers, we can be considered the first line of defense against airborne infections. The choices we make today will define the safety and well-being of countless individuals in the future. It is our duty to protect the public and we must take that responsibility seriously.


