Automation and controls systems at hospitals and health care facilities are changing

Respondents:
- Mark Chrisman, PE, PhD, Healthcare Practice Director, Principal, Henderson Engineers, Lenexa, Kansas
- Mike Fialkowski, PE, RCDD, LEED AP, Technology Services Market Leader, Affiliated Engineers Inc, Madison, Wisconsin
- Zach Frasier, PE, Mechanical Engineer, Moses Engineering, Gainesville, Florida
- Steve Lutz, PE, LEED AP, Associate Director, Harris, St. Paul, Minnesota

Mike Fialkowski, PE, RCDD, LEED AP, Technology Services Market Leader, Affiliated Engineers Inc, Madison, Wisconsin
Zach Frasier, PE, Mechanical Engineer, Moses Engineering, Gainesville, Florida
Steve Lutz, PE, LEED AP, Associate Director, Harris, St. Paul, Minnesota
From your experience, what systems within hospitals, health care facilities and medical campus projects are benefiting from automation that previously might not have been?
Mark Chrisman: With ongoing staff shortages, focusing on automating maintenance calls and alerts in leu of general alarms has been beneficial.
Mike Fialkowski: The systems that support location awareness (real-time location systems, RTLS and radio-frequency identification, RFID) will be a fundamental infrastructure in future facilities. Health care users have seen the benefit of specific systems (equipment tracking, inventory monitoring) to have situational awareness, but a unified infrastructure that supports multimodal location awareness will become the expectation. Location awareness will know when staff, patients, supplies and equipment are ready. Data generated can be used to enable meaningful process improvements and on-the-fly adjustments. Selection and implementation of a unified location awareness system is critical to the future state of providing care.
Zach Frasier: The transition to active direct digital control from pneumatic controls has been a mixed bag of success. Building automation system front-end monitoring has allowed latent issues that would not have been detected with a pneumatic system or even a standalone BAS to be detected. These issues have existed in some facilities for upward of 70 years. If there was no appreciable difference in hospital acquired infection rates, was detecting this issue really moving the patient care forward in that facility? On the other hand, DDC BAS are beginning to suffer serious sensor failures, which then disable the functionality of the BAS and leave the HVAC system less capable than it would have been with a pneumatic system while also measurably reducing the protection to the patient offered by the environment of care.
What types of system integration and/or interoperability issues have you overcome for these projects and how did you do so?
Mark Chrisman: The interconnection between audio-visual, fire alarm, security and nurse call is always difficult. We use a centralized set of interoperability drawings to help to make integration quicker and more efficient.
In what way is the need for more smart technology and features in such buildings affecting your work on these projects?

Mark Chrisman: Many owners currently don’t have the budgets to implement all the smart technology they would like within their projects. We strive to provide the infrastructure to make implementation possible down the road, which helps ensure the facilities we work on are future-proof.
Mike Fialkowski: Successful health care technology planning requires input from more stakeholders, better understanding of operational requirements, patient input data collection and acknowledgement of project budgets. Our health care technology teams need to continuously learn and share information to enable alignment of project specific designs with the technologies that will be available for the first patient. Selecting smart systems and technologies also requires a team that can identify requirements and problems to be solved, then select solutions, not the other way around. We bring cutting edge ideas to health care users to inspire creativity, but also need to be a filter for identifying viable solutions. All technologies need to be evaluated against project-specific requirements, tested for interoperability and supportable by the client. Without these fundamentals in place, technology planning will come up short.
Has the “internet of things” come up in discussion or been implemented on such projects? How has this integration impacted the project? If so, please give an example.
Mike Fialkowski: Health care projects have been dominated by connected devices due to the diversity of systems necessary and the complexity of patient care. Wearable sensors, personalized space control, interactive voice engagement and capacity for current and future IoT devices is a topic of conversation for every inpatient health care project. No single solution can be applied to all facilities. One key domain to manage is identifying wired vs wireless connectivity.
Ambulatory projects are candidates for more wireless computing devices as they have less patient monitoring wireless spectrum need. From prior project experience, this approach allows additional flexibility where devices are used on the wireless network, but often requires updating the budget to shift some wired network costs into funding a mission critical wireless network. For a specific client, the capacity of this network gave them more confidence that guest and IoT devices on the wireless infrastructure would not cause a future issue. On the inpatient side, the opposite condition dominates. Wireless spectrum is at a premium, so where devices are fixed, they should be connected to wired infrastructure. The wireless network still needs to be mission critical and any systems that can be wired will reduce the wireless load.
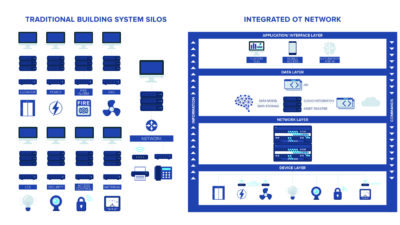
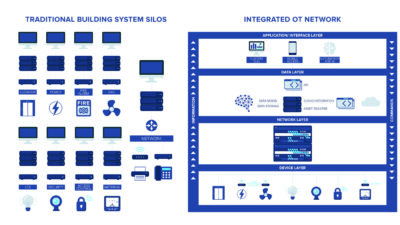
Zach Frasier: IoT has been a problem for the hospitals. IoT requires a network access, which poses a serious HIPAA security risk to the hospitals. As a result, many facilities have opted to install a separate IT backbone for the BAS. This effort has been expensive and problematic as most health care facilities are 20 to 60 years old and were not designed to accommodate extensive data cable trays in the above ceiling space nor the telecom switching rooms necessary.
Cybersecurity and vulnerability are increasing concerns. Are you encountering worry/resistance around wireless technology and IoT as the prevalence of such features increases? How are you responding to these concerns?
Mike Fialkowski: Implementing wireless transport layers that meet modern-day standards helps alleviate potential security vulnerabilities. Today’s focus needs to be on systems that will be on both the facility network and interact with authorized facility users. The vulnerability of these systems comes when they are not treated like enterprise IT systems. Each system we propose to touch a health care network needs an owner, a cybersecurity analysis, a deployment checklist, a connectivity/port audit and a maintenance plan. Health care chief system information officers expect that the due diligence and hardening of enterprise IT encompasses all other systems using the network for integration or intersystem connectivity.
Zach Frasier: Yes, we are. In the facilities that we work in their IT department have stipulated that no wireless devices are to be integrated into any network owned by the facility. Provision for network or internet access for MEP systems, where required has been provided by separate physical IT backbone that is isolated from the main hospital network.
How has your technology team worked with facility managers to implement security technology in hospitals, health care facilities and medical campuses?
Mark Chrisman: Our technology team coordinates with facility managers to determine the proper technology and locations for security measures. Providing security for staff during off hours and monitoring all possible patient entrance locations is critical, especially during staff shortages.
Zach Frasier: This is currently being developed with the facilities at which we work. The facilities we have automated are opting to move away from dedicated security systems, as those systems are being declared obsolete by the manufacturers and are no longer supported. The hospitals have opted to leverage the BAS platform to provide security, access and monitoring via the BAS.
What are some key differences in electrical, lighting and power systems you might incorporate in this kind of facility, compared to other projects?
Mike Fialkowski: Health care projects have always been candidates for centralized uninterruptible power supply to support IT loads. This becomes more pressing as systems beyond IT become considered mission critical by staff. Centralized UPSs may be expected to support systems that mirror the uptime of core IT: patient monitoring and notification systems, wireless networks supporting clinical communication, critical and sensitive imaging equipment and computer workstations that provide functionality should there be a connectivity issue.
In aggregate, these systems must be factored into the centralized UPS size and configuration. We consider a comprehensive analysis that looks at loads, resiliency and the operational cost of supporting equipment-specific UPS, critical to a responsible UPS design.