Critical facilities, such as health care buildings and hospitals, require fire alarm and detection specifications at a higher level than in other buildings.

Learning objectives
- Know the codes and standards that dictate fire alarm and detection.
- Understand fire alarm and detection requirements as specifically related to health care occupancies.
- Learn about fire alarm and detection in ambulatory health care facilities and assisted-living facilities.
Critical facilities, such as hospitals and nursing homes, require protection using an increased level of fire alarm and detection compared to many other types of facilities. Most of the fire alarm requirements are directly related to patient care or emergency procedures; however, some requirements are related to the unique nature and large areas in critical-care facilities. Health care occupancies are the portions health care facilities, such as hospitals and nursing homes, where occupants are incapable of self-preservation and are treated on an inpatient basis. The term “health care facilities” also includes ambulatory health care facilities, clinics, doctors’ offices, and portions of assisted-living facilities.
This article will reference the following codes and standards and how they relate to health care facilities:
- NFPA 72: National Fire Alarm and Signaling Code, 2013 edition
- NFPA 99: Health Care Facilities Code, 2015 edition
- NFPA 101: Life Safety Code, 2015 edition.
Note that Centers for Medicare & Medicaid Services (CMS) and the various accrediting organizations that certify and accredit health care organizations currently use the 2000 edition of NFPA 101. There are some differences between the 2000 and 2015 editions of NFPA 101 with respect to fire alarm and detection requirements, with increasing requirements for such systems in more recent editions of NFPA 101.
Zoning
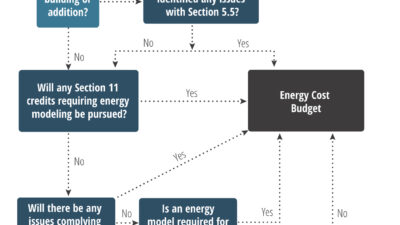
Zoning of fire alarm systems is critical in health care occupancies. It helps facility personnel determine where a potential fire incident is occurring, and assists the fire department in finding a fire. The best design practice for these facilities is to match the fire alarm zones to the smoke compartments. Smoke compartments are created in health care occupancies to establish temporary areas of refuge involving the horizontal relocation of patients/residents by dividing most stories into compartments of 22,500 sq ft or less. The zoning of sprinkler systems should also be consistent with smoke compartment and fire alarm zones. Further zoning of the fire alarm zone is also possible depending on the nature of departments in a smoke zone. For example, the smoke zone could be broken down into two different fire alarm zones if there are two unique departments in that smoke zone (see Figure 1).
Fire alarm zoning is permitted to be coordinated with sprinkler zones (NFPA 101, Paragraph 9.6.7.4.2) for all occupancies. In health care occupancies, fire alarm zones are permitted to coincide with smoke compartments (NFPA 101, Paragraph 18.3.4.3.3.2). In addition, NFPA 99 (Paragraph 15.7.4.3.1) specifically requires that all smoke zones and fire alarm zones be coordinated. As such, emergency control functions can be programed to coincide with the emergency plans that are based upon the smoke compartmentation within the facility.
Most modern fire alarm systems for large health care occupancies use addressable fire alarm initiating devices. As such, the programming of control functions by smoke compartments is a relatively simple activity. Zoning notification appliances per zone can be more difficult, but is often desired if notification occurs by zones, e.g., when selective notification concepts are to be used. If notification appliances are to be zoned, the devices must be wired independently by zone or more recent technology involving addressable notification devices must be used.
Notification
Fire alarm notification appliances have evolved drastically over the years. Older fire alarm systems only used electronic bells or chimes, and older health care occupancies typically used a coded notification signal to identify the zone or device in alarm. Strobes are also necessary to make the building compliant with accessibility requirements. NFPA 72 also requires strobes in all public spaces, assembly areas, and as needed in other parts of a health care facility.
Most modern fire alarm systems in health care occupancies are equipped with speakers that can multitask by providing both automated emergency communication messages and live messaging. Such technology also is easier to use in conjunction with coded messages such as “Code Red, Floor 3, East Wing” to provide increased information to facility staff without alerting patients, residents, and visitors.
Speakers for emergency communication systems are required where zoned or delayed egress procedures are desired (NFPA 72, Paragraph 24.4.2.8.2,). In addition, emergency voice/alarm communications systems are required for all high-rise buildings (NFPA 101, Paragraph 11.8.4.1).
Fire alarm speakers also can be used as a mass notification system (MNS). These systems are designed to broadcast more information than just a standard fire alarm system. Their capabilities include automated and live messages for weather emergencies, shooter events, bomb threats, or other events where communication to buildings occupants is desired.
Corridors
There are limited requirements for smoke detectors in corridors of health care occupancies due, in part, to a mandate to provide automatic sprinkler protection throughout new health care occupancies. However, smoke detectors often are required in areas open to the corridors and, in some instances, smoke detectors may be required in corridors when some spaces are open to the corridor (NFPA 101, Paragraphs 18.3.4.5.2 and 18.3.6.1(1)(c)). These can include stretcher storage areas, charting alcoves, or waiting areas. Nurses’ stations that are constantly occupied do not require smoke detection, and are considered to provide supervision to all areas within view of the station.
Nursing homes are required to have complete smoke detection in corridors in addition to spaces open to corridors (NFPA 101, Paragraph 18.3.4.5.3). Alternatively, smoke detection may be provided inside each sleeping room or self-closing devices with integral smoke detectors may be provided on patient-room doors.
Suites
Suites are a group of rooms that interconnect for facility operations and do not require any smoke-resistive walls within their boundaries (see Figure 2). Most standard suites do not require smoke detection. However, there are smoke-detector requirements if the suites are hazardous areas, are of a certain size, or have spaces that cannot be visually observed from the nurses’ station.
Hazardous areas include but are not limited to boiler rooms, paint shops, soiled linen rooms, and trash collection rooms. Sleeping suites between 7,500 and 10,000 sq ft require smoke detection throughout the suite (NFPA 101, Paragraph 18.2.5.7.2.3(C)(2)). Suites that have smoke-detection requirements must have smoke detectors throughout the entire space. Note that the 2000 edition of NFPA 101 does not have provisions for sleeping suites in excess of 5,000 sq ft in area.
Door magnetic release
There are numerous fire- and/or smoke-rated door requirements for health care occupancies. These rated doors must remain closed in an emergency to be effective. Self-closing doors can interfere with normal facility operations such as wheeling gurneys through such doors. To remedy this problem, the doors may be automatic-closing by smoke detection. The device holding such doors open releases and the door becomes self-closing based upon a signal from a smoke detector in the vicinity of the door being held open.
Though it is common practice to have one detector on each side of the door opening, it is possible to install one smoke detector on one side of the rated door, depending on the door header elevation and difference in height on each side.
There are two options available for health care occupancies when connecting hold-open devices to the fire alarm system. The smoke detectors in the vicinity of the door, as well as the fire alarm system and sprinkler water flow, must result in automatic-closing doors becoming self-closing either by smoke compartment or throughout the facility (NFPA 101, Paragraph 18.2.2.2.8). Again, this should coincide with the facility’s emergency plan. It should be noted that this is more restrictive than what is permitted by NFPA 72.
Locking arrangements
Doors are often locked in health care facilities to control security or to meet the clinical needs of the patients/residents. Three main areas that are in this category in health care facilities are operating areas, behavioral health units, and labor and delivery departments. These areas present unique concerns in relation to locking provisions and egress.
Operating areas are locked to keep people out for infection control. If an operating area takes up a large portion of a floor, this arrangement often can be an impediment in the means of egress. Thus, the means of egress must be designed to allow people to exit around the area or to pass through the area under special conditions.
Behavioral health units are designed to prevent patients from leaving a certain portion of their health care occupancies. This security is required for patient and other building occupant safety. Due to these concerns, behavioral health units must be designed to allow patients to egress from, or others to egress through, their portion of the facility despite the special security conditions.
Labor and delivery departments are designed with concerns regarding security issues for the patients (for example, baby theft) and infection control. Special locking arrangements are used to prevent newborns from being taken from the department without proper authorization. Access control is used to control infection, which is done by locking doors to prevent unauthorized entrance into the department. Beyond these arrangements, egress out of the department is free except for when a newborn baby with a secure armband approaches, which causes the doors to lock.
Two possible ways of providing safe egress and security is through “delayed-egress locks” (NFPA 101, Paragraph 7.2.1.6.1) and “access-controlled egress doors” (NFPA 101, Paragraph 7.2.1.6.2). Both of these arrangements require unlocking upon any fire alarm signal. The delayed-egress arrangement requires door hardware that sounds a local audible alarm when pressed, with the door opening within 15 sec. The access-controlled arrangement requires a motion detector to unlock the door as well as a “push to exit” button. These arrangements are not specific to health care occupancy, and can be used in most occupancies.
In addition to the above locking options, NFPA 101 allows a special locking arrangement unique to health care occupancies (Paragraph 18.2.2.2.5.2). This locking arrangement is allowed in special-care areas where patient needs require specialized security measures for their safety. These locks are required to unlock upon fire alarm activation or loss of power, and only one locking device is allowed per door. Additionally, all staff members must carry keys upon them at all times. Lastly, there must be either complete smoke protection throughout the locked space or a constantly attended location within the locked space from which the doors can be unlocked.
These locking arrangements require interfacing with the fire alarm system. At a minimum, fire alarm systems must monitor the smoke detectors typically required as part of the special locking arrangements. At the other extreme, fire alarm systems can control the whole process depending on how the locking arrangements are installed and programmed. Before such door-locking arrangements are installed, compliance with the applicable fire alarm requirements must be verified
As there are many components that go into making a door-locking arrangement compliant, coordination between trades is critical. Within health care occupancies, all locks, egress, detection, alarms, and emergency planning come together to create a safe environment for all of the building’s occupants.
Other fire alarm requirements
Manual fire alarm boxes provide an additional level of detection by allowing occupants to initiate the fire alarm. In patient sleeping areas there are provisions that allow the omission of fire alarm boxes at each exit, provided manual fire alarm boxes are installed at a constantly attended location, are continuously accessible and visible, and are within required travel distances. This allows more control over accidental alarms while still providing a manual alarm initiation option.
Sleeping rooms without direct access to an exit access corridor, e.g., egress through an “anteroom”, are only allowed where smoke detection is provided in the anteroom (NFPA 101, Paragraph 18.2.5.6.2). This arrangement provides additional notification if the only means of egress from the sleeping room might become blocked by a fire.
Interfaces with suppression systems
Health care facilities often have large footprints, are multiple stories, and have unique uses within various parts of their buildings. Thus, fire alarm systems must perform several unique functions in health care facilities that are not directly connected to patient care. Some of these items include interfacing with suppression systems such as wet pipe sprinkler systems, preaction sprinkler systems, and gaseous suppression systems
All new health care occupancies are to be protected with supervised automatic sprinkler systems (NFPA 101, Paragraph 18.3.5.1). The fire alarm system must monitor all control valves, flow switches, fire pumps, kitchen suppression systems, and other necessary sprinkler and water supply components. Thus, detailed coordination is necessary to determine the total number of interface devices.
Preaction sprinkler systems provide a unique challenge. They are intended to prevent the unnecessary discharge of fire-suppression water in rooms with equipment of high value. In a single interlock preaction sprinkler system, water enters the sprinkler system pipes when a detector activates. Beyond this, the water will not be discharged from the system until a sprinkler activates, and it will only release water from the activated sprinkler(s). When such a system is used, the fire alarm system controls the actuation of the sprinkler system. In such situations, the fire alarm panel must be listed for fire-suppression releasing service. As an alternative, a single, dedicated releasing panel can be provided in lieu of using the main fire alarm control panel for releasing service. Installing a sub-panel minimizes coordination with the main fire alarm system, but requires additional maintenance; and the sub-panel must be monitored by the building’s fire alarm system.
Most gaseous suppression systems are custom-built packages with integrated releasing panels and detection systems. However, these sub-panels must be designed and maintained just the same as the main fire alarm system. Additional concerns for gaseous suppression systems include pre-discharge alarms and bypass switches for maintenance. All of these items must be properly coordinated. Lastly, the gaseous-suppression sub-panels must be interfaced to the main fire alarm system with at least an alarm and supervisory signal.
Other interfaces, facility types
Many hospitals have places for staff sleeping or “on-call” rooms. Whereas such spaces are considered a residential occupancy, these rooms must be provided with smoke alarms. Although not required, the smoke alarms are permitted to be connected to the building fire alarm system.
Ambulatory health care facilities are facilities where occupants are incapable of self-evacuation and are treated on an outpatient basis. The detection requirements for ambulatory health care facilities focus on prompt detection by staff or automatic detection, swift occupant and emergency forces notification, and sprinkler protection. Ambulatory health care facility requirements are based upon requirements for both business occupancies and health care occupancies. As an alternative to smoke compartments within the facility, 5,000-sq-ft areas with smoke detection throughout are permitted (NFPA 101, Paragraph 20.3.7.2).
Assisted-living facilities encompass two or more different occupancy classifications, typically including health care and residential board and care. Portions of an assisted-living facility classified as a health care occupancy (nursing home) need to comply with the provisions discussed above. Areas of an assisted-living facility in which personal care is provided shall meet the requirements for a residential board-and-care occupancy. Other areas, such as independent living accommodations, may be classified as a residential occupancy.
Ensuring success
Even the best-installed fire alarm system is of little benefit without proper training and procedures to implement during an evacuation to control the facility’s occupants. The alarm notifies the staff of the health care occupancy, indicating that the emergency plan needs to be implemented. While NFPA 101 contains emergency planning, fire drill, and training requirements, individual health care facilities need to determine how to best implement training procedures and use the fire alarm system. Ensuring that staff members understand the fire emergency procedures in a health care occupancy is essential to providing safety to those within their buildings.
Critical facilities, such as health care occupancies, require fire alarm and detection requirements at a higher level than in other buildings. These requirements are crucial in providing an acceptable level of life safety for the occupants in these critical-care facilities
William E. Koffel is president of Koffel Associates. He is chair of the NFPA Correlating Committee on Life Safety and a member of numerous 72 and NFPA 101 technical committees. He is a member of the Consulting-Specifying Engineer editorial advisory board. M. Steven Welsh is a registered fire protection engineer at Koffel Associates. He has extensive design and construction period service experience with major projects involving health care, hazardous materials, high rises, business, assembly spaces, and university complexes. Kristin Steranka has been an engineering technician at Koffel Associates. She graduated from the University of Maryland in May 2015 and started as a fire protection engineer at Koffel Associates in June.