Specifying engineers discuss automation considerations and important codes for hospitals and health care facilities

Health care insights:
- The integration of smart technologies in health care facilities enhances patient care and operational efficiency.
- Adherence to codes and standards like NFPA, FGI, and ASHRAE ensures compliance and safety, but understanding jurisdiction-specific interpretations is key to effective implementation.
Respondents:
- Cory Duggin, PE, LEED AP BD+C, BEMP, Principal / Senior Energy Wizard, TLC Engineering Solutions, Brentwood, Tenn.
- Benjamin Medich, PE, Vice president, HDR, Pennington, N.J.
- Daniel Noto, PE, LEED AP, Southeast market leader, Fitzemeyer and Tocci Associates, Alpharetta, Ga.
- Kevin Jayne, PE, LEED AP, Principal. Affiliated Engineers, Inc., Denver, Colo.
From your experience, what systems within hospitals, health care facilities and medical campus projects are benefiting from automation that previously might not have been?
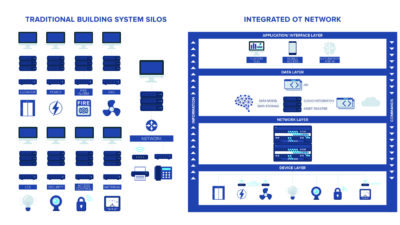
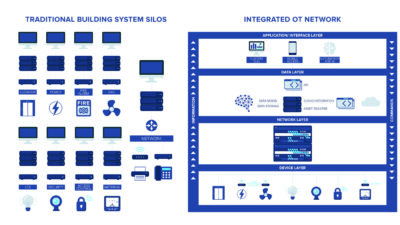
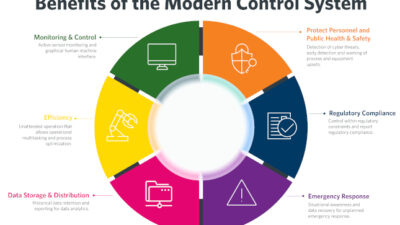
Kevin Jayne: Rapid advancements in technology and computing power continually equip modern hospital facilities and caregivers with greater access to information. There’s been an industry movement towards telemedicine for many years, a trend that accelerated during the pandemic; these systems now offer enhanced capabilities, providing patients with more immediate access to quality care. Infrastructure to support patient monitoring services has become essential in modern patient rooms. New engineering systems typically integrate with building automation system networks, enabling continuous data logging, supporting improved analysis, and offering predictive insights for facility staff.
What types of system integration and/or interoperability issues have you overcome for these projects and how did you do so?
Kevin Jayne: Smart technology enables clinical, IT, and facilities staff to streamline operations in modern healthcare settings. Given the growing number of stakeholders and subject matter experts involved, integrating these advanced systems necessitates a strategic and collaborative approach. To fully leverage smart technology’s potential, comprehensive system analysis is essential, including infrastructure planning for future upgrades.
Cybersecurity and vulnerability are increasing concerns. Are you encountering worry/resistance around wireless technology and IoT as the prevalence of such features increases? How are you responding to these concerns?
Benjamin Medich: As cybersecurity and vulnerability concerns grow, we typically restrict the use of wireless technology and prioritize strong cybersecurity measures in our equipment specifications. Our team of dedicated cybersecurity engineers design comprehensive protection schemes to safeguard systems.
However, wireless systems inherently present additional entry points for potential cyber threats. While network segmentations can help maintain network integrity and limit the risk of bad actors compromising IoT devices, the inability to maintain current security protocols in many IoT devices is challenging; in many instances, the potential risk outweighs the benefit.
Please explain some of the codes, standards and guidelines you commonly use during the project’s design process. Which codes/standards should engineers be most aware of?
Kevin Jayne: In addition to the suite of International Building Codes that govern various aspects of commercial buildings, health care design must adhere to other sets of codes and guidelines that require careful review and understanding for proper application. The Facility Guidelines Institute (FGI) encompasses ASHRAE Standard 170: Ventilation of Health Care Facilities, which dictates numerous engineering requirements, including quantity and type specifications for electrical, medical gas and low voltage devices, along with mechanical system requirements related to temperature, air changes and pressure relationships. A health care designer must be familiar with FGI to effectively apply relevant design concepts across a range of programmatic applications.
Benjamin Medich: The cornerstone of design is NFPA 99: Health Care Facilities Code, NFPA 70: National Electrical Code (NEC) and FGI. While NFPA 70 and 99 carry the force of code through adoption, FGI’s authority currently stems from its use by the Joint Commission in evaluating facilities. NFPA 70 and NFPA 99 are not always aligned, and it is important to know where they diverge, including selective coordination requirements. It’s also necessary to know how your local authority having jurisdiction (AHJ) is interpreting these requirements. For example, many jurisdictions default to the NFPA 99 requirement for selective coordination in hospitals, while some others use the more stringent NFPA 70 requirements.
What are some best practices to ensure that such buildings meet and exceed codes and standards?
Kevin Jayne: Proper code application begins with familiarity, as any early design oversight can lead to significant ramifications later in the project. On large-scale projects, the code cycle may shift to the next iteration mid-design, requiring the design engineer to stay current with industry trends. For instance, the FGI 2022 introduced additional resiliency standards through a mandated Disaster, Emergency and Vulnerability Assessment, placing greater emphasis on disaster preparedness than what had been covered historically through the Safety Risk Assessment. A thorough understanding of this process enables health care designers to guide the owner through the assessment and deliver system designs that align with the owner’s goals.

Daniel Noto: For me, the first step is understanding the standards and codes. This comes from referring to them during design, but also staying involved in professional organizations that write the standards (i.e., ASHRAE). From there, one needs to understand that standards and codes are the absolute least you can do on a project. Designing above those standards and codes is key to a truly successful project and a health care facility that operates with a higher standard of performance.
Benjamin Medich: First and foremost, it is essential to read and understand the codes. This involves understanding the content that is written, and also how your AHJ and hospital administration interpret these codes. Depending on your location, interpretation can vary. For example, do you need isolation panels in the operating room (OR)? This depends on whether the OR is designated as a “Wet Procedure Location” according to NFPA 99. However, NFPA does not directly define a “Wet Procedure Location,” this designation is made by the hospital. Understanding these types of code variations and interpretations will streamline your approach to designing the facility. Conducting code reviews throughout the design process also keeps the design team updated on emerging regulations that may need to be applied to the project, or which may be beneficial to incorporate.
How are codes, standards or guidelines for energy efficiency impacting the design of such projects?
Kevin Jayne: Each International Energy Conservation Code iteration typically raises the target benchmarks significantly, meaning progressive design decisions and system types that may have been considered selective or optional in the past, are now becoming requirements. Heat recovery chillers exemplify this trend; meeting the current energy codes all but necessitates using a heat recovery chiller to address the coincident base heating and cooling loads in hospitals year-round. At the local level, state and city building code programs further accelerate decarbonization by implementing benchmarks and imposing financial penalties for non-compliance.
Benjamin Medich: Several codes, standards and guidelines apply to various aspects of health care facilities. Professionals must first verify which codes have been adopted and are currently in effect. Additionally, it is essential to determine if the client has any facility standards that must be adhered to. These standards and guidelines help guide design decisions, however, conflicting requirements can arise, which may complicate and slow down the process. Navigating these conflicts requires careful coordination and a thorough understanding of both regulatory and client-specific requirements to achieve a compliant and efficient design.
In general, what issues are newer codes and standards working to address?
Benjamin Medich: The FGI will be amending its publications to more formally separate code required elements from recommended practices. ASHRAE Standard 90.1: Energy Standard for Buildings Except Low-Rise Residential Buildings will update occupancy control requirements to formally include an exclusion for some patient care areas.