NFPA 99-2015 has a few changes that mechanical engineers should pay close attention to.
Learning objectives
- Identify major changes to the 2015 edition of NFPA 99: Health Care Facilities Code that impact mechanical designers.
- Learn to build upon the risk-based approach of NFPA 99 when designing hospitals and health care facilities.
NFPA 99: Health Care Facilities Code applies to all health care facilities other than home care. The code is intended for professionals involved in the design, construction, maintenance, and inspection of health care facilities in addition to the design, manufacture, and testing of appliances and equipment used in patient-care rooms of the health care facilities.
NFPA 99-2015 continues to build upon the risk-based categories established in the 2012 edition. As many health care designers are aware, the 2012 edition of NFPA 99 experienced a major overhaul. The intent of the upgrade was to elevate NFPA 99-2012 from a standard to a code, allowing it to be incorporated into a local jurisdiction’s code by itself instead of being referenced from NFPA 101: Life Safety Code.
The 2012 edition eliminated all previous occupancy-based chapters and replaced them with Chapter 4: Fundamentals, which established risk categories 1 through 4. The change meant NFPA 99 would no longer be applied based upon the name of an occupied space, but rather applied based upon a risk category. Unchanged in the 2015 edition, the risk category is determined by the impact of system failure on patients and caregivers within a facility space. The higher the risk to occupants in the event of system loss, the stricter the requirements to ensure the system is not lost.
While the overall structure and majority of the content remain the same between the 2012 and 2015 NFPA 99 editions, slight modifications have been made throughout the code in the latest version. The changes in the 2015 edition that are of most importance to a health care mechanical designer appear in Chapter 5: Gas and Vacuum Systems; Chapter 7: Information Technology and Communications Systems; and Chapter 9: HVAC. Chapter 8: Plumbing, which was added in the 2012 edition of NFPA 99 with the intent that it be used to support the local plumbing codes for health care facilities, has not been modified in the 2015 edition.
Chapter 5: Gas and vacuum systems
As in the 2012 edition, NFPA 99-2015 divides Chapter 5 into three sections corresponding to Category 1, Category 2, and Category 3 systems.
Category 1 systems are the most critical and are required to be available continuously for patient life support, even during the loss of normal power sources or failure of other hospital systems. It is important to note that Chapter 5 does not include a Category 4 system (no impact on patients) because a failure of a gas and vacuum system would have at least some impact on the patient. The minimum risk level for a gas and vacuum system, therefore, is Category 3 (failure may cause discomfort).
NFPA 99-2015 adds new criteria in Chapter 5 to help define a Category 1, Category 2, and Category 3 piped gas and vacuum system. The intent of the change is to ensure that when a facility is performing a risk assessment as defined in Chapter 4, the risk assessment is not being used to lower the level of safety. For example, prior to the 2015 edition, it may have been possible for a facility performing a risk assessment to define a medical-gas system as Category 2 even though deep sedation was administered to the patient. Because of the changes to the 2015 code, this situation would now be required to be classified as Category 1.
The added language in Chapter 5 of the 2015 edition is to be used in addition to the risk-category definitions in Chapter 4 when conducting the risk assessment of a facility’s gas and vacuum systems.
Other updates in Chapter 5 affect storage temperatures, auxiliary-source connections, master medical-gas alarms, and instrument air.
For all three categories of medical-gas systems under section 5.1.3.2.12, the 2015 code changed the maximum storage temperature of gas cylinders from 130° to 125°F to match the Compressed Gas Association recommendations. Under section 5.1.3.2.13, the 2015 edition also has modified the minimum storage temperature for nitrous oxide and carbon dioxide cylinders from -20° to 20°F.
Section 5.1.3.5.7, Auxiliary Source Connection, was added in the 2015 edition for medical-gas systems. The section states, “All source systems shall be provided with an auxiliary source connection point of the same size as the main line, which shall be located immediately on the patient side of the source valve.” The section further stipulates that the connection shall consist of a tee and a normally closed secured valve (see Figure 1). The intent of this addition is to provide a facility with a simpler and safer means to change out service equipment. It is important to note that this additional source requirement does not modify or remove the requirements of the emergency oxygen-supply connection referenced in Section 5.1.3.5.15. This section remains unchanged from the 2012 edition.
Section 5.1.9.2.3, Master Medical Gas Alarm, was revised to differentiate between the wired and wireless communication between the two mandatory master alarm panels and the initiating device. Under either wired or wireless communication, the intent of the code remains unchanged: that should one of the mandatory master alarm panels fail, its failure does not disable any signal on the other mandatory master alarm panel.
NFPA 99-2015 also has added a dedicated section for instrument air under Section 5.1.13, Category Support Gases. This section was added to avoid the confusion between nitrogen, which is a medical gas, and instrument air, which is a support gas. Instrument air is not mandated to be provided, but when it is provided, it shall comply with the requirements of NFPA 99.
Furthermore, when support equipment, such as operating room booms or control panels, require gas to operate, a facility has the option of providing either instrument air or nitrogen. However, because it is uncommon and usually unnecessary for a facility to use both an instrument air system and a nitrogen system, NFPA 99 recommends a decision be made to use the one system that best meets the facility’s needs.
Chapter 7: Information technology and communications systems
NFPA 99-2015 introduces one change of importance to mechanical designers in Chapter 7, which was added in the 2012 edition and is divided into three risk categories.
The change alters restrictions for the routing of utilities through a Category 1 telecom entrance facility (EF) and technology equipment room (TER). The 2015 edition eliminates the 2012 requirement that underground utilities, such as electrical, water, gas, and sewer, could not be located below a Category 1 EF. As in 2012, however, Sections 7.3.1.2.1.4 and 7.3.1.2.2.4 of the 2015 edition continue to stipulate that mechanical equipment of any kind that does not directly serve the TER or EF shall not be installed in, pass through, or enter the space. (This type of restriction is similar to those found in the international codes for nonessential utilities routed within egress stairwells or elevator machine rooms.)
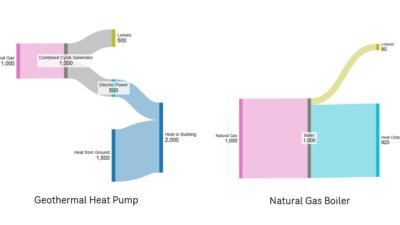
Chapter 7 also maintains the requirement that an EF or TER must have a positive pressure differential with respect to surrounding areas. Under the “environmental requirements” in Section 7.3.1.2.1.8, a designer must provide a means for maintaining a positive air pressure relationship for the technology space. Attention must be paid to ensure this pressure relationship is maintained when dedicated terminal heat-transfer units are provided (see Figure 2).
Chapter 9: HVAC
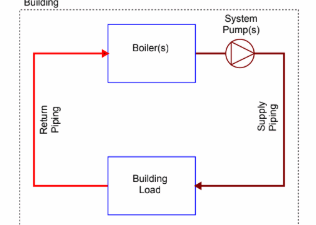
Unlike chapters 5 and 7, the HVAC section does not define systems based upon a risk category. The section requires each facility to perform a risk assessment to assign a risk category in accordance with Sections 4.1 and 4.2. Similar to the 2012 edition, NFPA 99-2015 is written with the intent that the risk category assigned to each HVAC system serving a space is independent of the risk category applied to other systems serving the same space.
For example, a central sterile supply located at a health care facility in Dallas may assign a risk category of 3 to the heating system serving the department, but assign a risk category of 2 to the cooling system. Assigning Category 3 to the heating system may be justified because, while the failure of the heating system may cause discomfort for the staff, its failure is unlikely to cause injury. Assigning Category 2 for the cooling system also would be reasonable because, should it fail, the inability to control humidity within the department may result in the failure of sterile products, which could cause minor injury to patients.
Chapter 5 points out that the facility has the responsibility for developing the risk assessment for its HVAC system. This allows flexibility in assigning risk to mechanical systems based on their specific equipment and their associated risk. The code’s intent is to not burden facilities with mandates on redundancy or major equipment upgrades. The process and the documentation for the HVAC system must be done by the facility as noted in Chapter 4, Section 4.2. The section does not specify the type of assessment the facility should conduct, but only states the assessment be a defined procedure that is documented.
A major change in Section 9.3.1.3 of the 2015 edition is very clear language that removes the requirement for smoke purge for HVAC systems in anesthetizing locations.
Prior to the 2012 edition, NFPA 99 required that anesthetizing locations be served by an HVAC system capable of removing smoke from the room without recirculating it through the system or returning it to the room it serves. This requirement added extra cost and complexity as designers specified smoke purge on any air-handling system that served anesthetizing locations, such as an operating room or catheterization lab. The smoke-purge system control sequence was such that if smoke was detected within the anesthetizing location, the air-handling system would go to 100% outside air, therefore relieving all air to the exterior and eliminating any opportunity for the smoke-filled air to be recirculated through the system or returned to the room it serves.
In northern climates, which commonly experience below-freezing temperatures, additional heating capacity is typically added to the air-handling system. Should the air-handling system experience a smoke-purge occurrence when outside-air temperatures are below freezing, the additional heating capacity is used to ensure the cold air is not distributed through the space and does not cause damage.
While the 2012 edition of NFPA 99 removed the requirement for smoke purge in anesthetizing locations, its deletion led to confusion in the industry as designers debated whether the removal was intentional. The 2015 edition has ended the debate by clarifying that smoke purge in anesthetizing locations is no longer required. The requirement for smoke purge in anesthetizing locations was established years ago when the use of flammable anesthetics was common in operating rooms and, therefore, the fire hazard was much higher. With today’s usage of nonflammable anesthetics, the fire hazard has been reduced, resulting in the definitive removal of the smoke-purge requirement in the 2015 edition.
Another change in Chapter 9 is the consolidation of Section 9.3.9, Emergency Power System Room. The 2012 edition included several paragraphs copied from NFPA 110: Standard for Emergency and Standby Power Systems. The 2015 edition has removed these paragraphs and simply states that all HVAC systems serving the emergency power system room shall be compliant to NFPA 110.
The 2015 edition of NFPA 99 did not experience major structural or content changes, but has made modifications to build upon the risk-based approach established in the 2012 edition. Due to NFPA 99’s application to a wide range of infrastructure, equipment, and design approaches for a health care facility, it is, therefore, critical for mechanical engineers to review the entire 2015 edition to have a complete understanding of the code’s latest requirements.
Mike Zorich is a client executive and leads one of IMEG Corp.’s health care design groups. He has served as a project manager and lead mechanical engineer for a wide variety of health care facilities and is adept at system concept and design for new greenfield hospitals, renovations, expansions, and infrastructure upgrades.